How I Turned My Fatty Liver Around – A Real Lifestyle Change Story
Fatty liver used to be my silent health crisis—no pain, no alarms, just a warning sign I ignored for years. Then I learned it could lead to serious damage if left unchecked. This isn’t a miracle cure, but a real, science-backed journey of lifestyle shifts that made a difference. I’ll walk you through what actually works, why it matters, and how small daily choices can protect your liver—naturally and sustainably. Always consult your doctor, but know this: change *is* possible.
The Wake-Up Call: Recognizing Fatty Liver
Fatty liver disease, particularly non-alcoholic fatty liver disease (NAFLD), affects nearly one in three adults worldwide, yet many remain unaware they have it. The condition occurs when excess fat builds up in liver cells—not due to alcohol, but often as a result of metabolic imbalances. It’s closely linked with insulin resistance, obesity, and high triglycerides, but even individuals at a normal weight can develop it. What makes it especially dangerous is its stealthy nature: most people experience no symptoms until significant damage has occurred. There’s no sharp pain, no obvious warning, just a gradual strain on one of the body’s most vital organs.
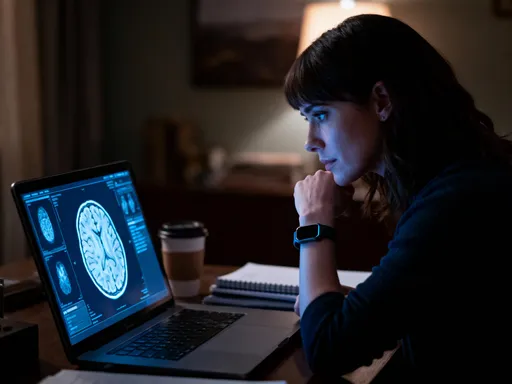
For me, the diagnosis came during a routine physical. My blood tests showed elevated liver enzymes—ALT and AST levels above the normal range. That prompted an ultrasound, which confirmed fat accumulation in my liver. At first, I was shocked. I didn’t drink heavily, I wasn’t overweight, and I considered myself relatively healthy. But the truth was, my diet was high in processed foods, I sat for long hours at work, and I rarely prioritized movement. My doctor explained that while medication wasn’t the first line of defense, lifestyle changes could significantly reverse the condition—if I acted early.
That moment was a wake-up call. I realized that waiting for symptoms to appear could mean waiting too long. The liver has an incredible ability to regenerate, but only up to a point. Left unaddressed, fatty liver can progress to inflammation (steatohepatitis), fibrosis, and even cirrhosis. The good news? In its early stages, it’s largely reversible through diet, exercise, and healthy habits. The key is intervention before irreversible damage sets in. My journey began not with a prescription, but with a commitment to understand my body and make meaningful, sustainable changes.
Debunking Myths: What Fatty Liver Isn’t
One of the biggest obstacles to addressing fatty liver is misunderstanding what it really is. Many people assume it’s a condition that only affects heavy drinkers or those who are visibly overweight. This misconception can lead to stigma, shame, and delayed action. The truth is, non-alcoholic fatty liver disease has nothing to do with alcohol consumption. It’s driven by metabolic dysfunction—how the body processes fats and sugars—and is increasingly common in people of all body types, including those with a normal BMI.
NAFLD exists on a spectrum. At its mildest, it’s simple fat accumulation (steatosis), which may not cause harm if managed. But in some cases, it progresses to non-alcoholic steatohepatitis (NASH), where the liver becomes inflamed and begins to scar. This is the stage that raises the risk of serious complications. What’s alarming is that up to 30% of people with NAFLD may develop NASH, and many don’t know until it’s advanced. The absence of symptoms doesn’t mean safety. In fact, fatigue, mild abdominal discomfort, or brain fog might be the only signs—and these are often dismissed as part of busy, stressful lives.
Another myth is that blood work will always catch it early. While elevated liver enzymes can signal trouble, they don’t tell the whole story. Some people with fatty liver have normal enzyme levels, especially in the early stages. That’s why imaging, like an ultrasound or FibroScan, is often needed for a definitive diagnosis. Relying solely on how you feel—or on a single blood test—can create a false sense of security. The reality is, fatty liver is a growing public health issue, tied to modern diets high in sugar and ultra-processed foods, sedentary lifestyles, and rising rates of insulin resistance. Recognizing it for what it is—a metabolic condition, not a moral failing—is the first step toward effective management.
Food That Fuels Recovery: What to Eat and Why
Diet is the cornerstone of reversing fatty liver, and the changes I made were both simple and powerful. The biggest shift? Cutting out added sugars and refined carbohydrates. This meant no more sugary cereals, white bread, pastries, or sweetened beverages—even fruit juices. These foods spike blood sugar and insulin levels, prompting the liver to convert excess glucose into fat. Over time, this process contributes directly to fat buildup in liver cells. By reducing my intake of these foods, I lowered the metabolic burden on my liver and gave it a chance to heal.
Instead, I focused on whole, unprocessed foods. I increased my intake of fiber-rich vegetables, legumes, and whole grains like quinoa and steel-cut oats. These foods stabilize blood sugar, improve insulin sensitivity, and support healthy digestion. I also prioritized healthy fats—avocados, nuts, seeds, and olive oil—which do not contribute to liver fat and actually support cell function. Protein became a consistent part of every meal, especially plant-based sources like lentils, chickpeas, and tofu, as well as lean animal proteins like eggs, fish, and skinless poultry. These helped maintain muscle mass and kept me feeling full, reducing the urge to snack on unhealthy options.
One of the easiest and most effective swaps was changing my breakfast. I used to eat a bowl of sweetened cereal with skim milk—high in refined carbs and low in fiber. Now, I have steel-cut oats topped with walnuts, chia seeds, and a few berries. This meal provides sustained energy, supports gut health, and reduces liver fat over time. Another change was cooking at home more often. Restaurant meals and packaged foods are often loaded with hidden sugars, unhealthy fats, and sodium. By preparing meals myself, I could control the ingredients and avoid unnecessary additives.
A typical day of eating now looks like this: breakfast with oats and nuts, a mid-morning snack of Greek yogurt with cinnamon, lunch with a large salad, grilled chicken, and quinoa, an afternoon snack of apple slices with almond butter, and dinner with baked salmon, roasted vegetables, and a small portion of sweet potato. This approach isn’t about deprivation—it’s about nourishment. Each meal supports liver function, reduces inflammation, and helps the body burn fat more efficiently. The results weren’t immediate, but over months, my energy improved, my cravings diminished, and follow-up tests showed a clear reduction in liver fat.
Movement as Medicine: Exercise That Works for Liver Health
If diet is the foundation, exercise is the scaffold that holds the recovery process together. I used to think that only intense workouts—long runs or high-intensity training—could make a difference. But research shows that even moderate physical activity can significantly reduce liver fat. The key isn’t intensity; it’s consistency. Regular movement improves insulin sensitivity, helps regulate blood sugar, and encourages the body to use stored fat for energy—including the fat in the liver.
I started with something simple: a 30-minute walk every day. At first, it was just around my neighborhood after dinner. Over time, I increased the pace and duration, eventually working up to 10,000 steps most days. Walking became a non-negotiable part of my routine, not just for my liver, but for my mental clarity and stress relief. What surprised me was how much even this modest activity improved my sleep and mood. But I didn’t stop there. I added two weekly strength training sessions using bodyweight exercises and light dumbbells. Building muscle increases resting metabolic rate, which means the body burns more calories even at rest—further supporting fat loss, including in the liver.
My weekly movement plan now includes five days of walking (45 minutes each), two days of strength training, and daily stretching or light yoga. I also try to stay active throughout the day—taking the stairs, parking farther away, standing while talking on the phone. These small efforts add up. Studies have shown that combining aerobic exercise with resistance training is more effective for reducing liver fat than either alone. The important thing is to find activities you enjoy and can stick with. It’s not about perfection; it’s about showing up, day after day. Over six months, these changes led to measurable improvements in my liver health, confirmed by follow-up imaging and blood tests.
Sleep, Stress, and the Hidden Liver Triggers
One of the most overlooked factors in liver health is sleep. I used to stay up late, scrolling through my phone or watching TV, thinking it didn’t matter as long as I got to bed eventually. But poor sleep disrupts hormones that regulate appetite and metabolism. When we’re sleep-deprived, levels of ghrelin (the hunger hormone) rise, while leptin (the satiety hormone) drops. This can lead to overeating, especially of high-calorie, sugary foods. More importantly, lack of sleep increases cortisol, the stress hormone, which promotes fat storage—particularly in the liver and abdomen.
Chronic stress, whether from work, family, or daily pressures, has a similar effect. Elevated cortisol over time contributes to insulin resistance and fat accumulation. I realized that my constant low-level anxiety wasn’t just affecting my mood—it was silently harming my liver. To address this, I began building small, sustainable habits to reduce stress and improve sleep. I set a bedtime alarm to remind me to wind down. I turned off screens an hour before bed and started reading or doing light stretching instead. I also began practicing deep breathing exercises for five minutes each morning and evening. These simple routines helped calm my nervous system and lowered my overall stress levels.
I also made my bedroom a sleep sanctuary—cool, dark, and quiet. I invested in blackout curtains and a white noise machine, which made a noticeable difference in the quality of my rest. On stressful days, I took short walks during lunch or practiced mindful breathing at my desk. These aren’t dramatic changes, but they create a cumulative effect. Over time, I noticed that I felt less reactive, slept more deeply, and had fewer late-night cravings. Research supports this: improving sleep quality and managing stress are associated with reduced liver fat and better metabolic health. Healing the liver isn’t just about what you eat or how much you move—it’s also about how well you rest and how you manage the invisible pressures of daily life.
Tracking Progress Without Obsession
When I first started this journey, I was tempted to monitor everything—my weight daily, my food intake down to the calorie, my steps every hour. But I quickly learned that obsession can backfire. Constant tracking can lead to anxiety, frustration, and even disordered behaviors. Instead, I shifted to a more balanced approach: tracking key indicators without becoming consumed by them. I focused on meaningful markers of progress, not just the number on the scale.
Energy levels became one of my most important signals. Within a few weeks of changing my diet and increasing movement, I noticed I wasn’t hitting that mid-afternoon slump anymore. I felt more alert, focused, and emotionally stable. My clothes fit better, and my waistline gradually decreased—two signs of visceral fat loss, which is closely linked to liver health. I also paid attention to my mood and sleep quality, both of which improved significantly. These non-scale victories were powerful motivators, reminding me that health is more than a number.
Medically, I scheduled follow-up appointments every three to six months. My doctor monitored my liver enzymes, fasting insulin, blood sugar, and triglycerides. Over time, these markers trended in the right direction. An ultrasound after one year showed a clear reduction in liver fat. But I didn’t check these numbers obsessively. I trusted the process and the gradual improvements. I also learned to accept setbacks as part of the journey. There were holidays, family events, and stressful weeks when I slipped back into old habits. Instead of giving up, I viewed these as temporary detours, not failures. The key was returning to my routine without guilt or self-criticism. Progress isn’t linear, but consistency over time yields results.
Making It Stick: Building a Liver-Healthy Life for Good
The most important lesson I’ve learned is that lasting change isn’t about short-term fixes—it’s about building a lifestyle that supports long-term health. Reversing fatty liver wasn’t a 30-day challenge or a drastic diet; it was a series of small, sustainable choices that became habits. I stopped thinking of it as a “liver diet” and started seeing it as a way of living that naturally supports my body’s needs. The habits I formed—cooking at home, walking daily, prioritizing sleep, managing stress—didn’t feel like sacrifices. They became part of my identity, woven into the rhythm of my days.
Of course, there were setbacks. I remember one family vacation where I ate more processed snacks and skipped workouts. When I returned, I felt sluggish, and my motivation dipped. But instead of abandoning the journey, I reminded myself why I started. I returned to my routine gently, without judgment. I’ve come to see setbacks not as failures, but as feedback—moments to reassess, adjust, and recommit. What matters is not perfection, but persistence. Over time, the positive changes compounded. My liver function improved, my energy soared, and I felt more in control of my health than ever before.
Today, I view my liver not just as an organ, but as a mirror of my daily choices. It doesn’t ask for grand gestures—just consistent care. It can heal, regenerate, and thrive when given the right support. This journey taught me that health isn’t something that happens to us; it’s something we create, one decision at a time. You don’t need a dramatic overhaul to make a difference. Start with one meal, one walk, one night of better sleep. Small choices, repeated over time, lead to real transformation. And if I can do it, so can you. Your liver is resilient. With patience, knowledge, and steady action, it *can* heal.